肺结节CT的征象及显示(综述)(图文)
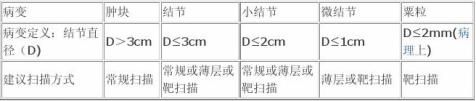
肺结节(pulmonary nodule)通常是指直径不超过3cm的肺内类圆形病灶,不超过2cm则称为小结节,其中不超过1cm可称为微结节(附表)。小结节病变的诊断和鉴别诊断一直是放射学的一个难题,如何提高小结节的细节(details)显示是其中的关键。俗语“巧妇难为无米之炊”,对于一个毫无特征可言的肺结节,再高明的医生也难下结论,而对一个特征详尽的肺结节,即使一个初验者也有同样准确的答案。随着螺旋CT的出现,小结节的细节显示和准确诊断率得到明显的提高。而如何最有效地显示结节特征(characterization)是提出准确诊断的前提。
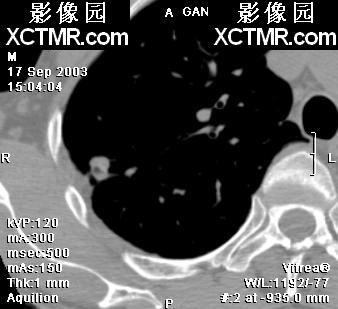
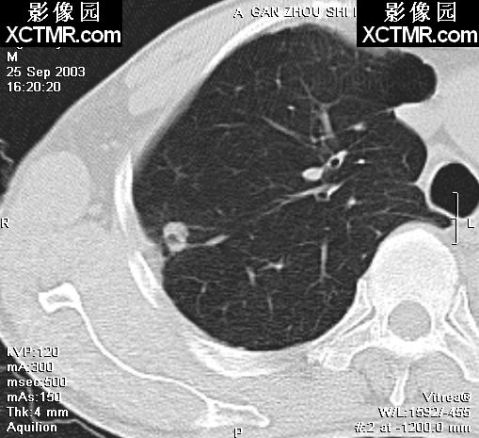
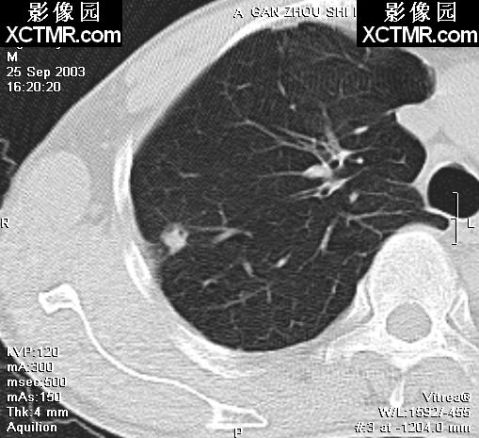
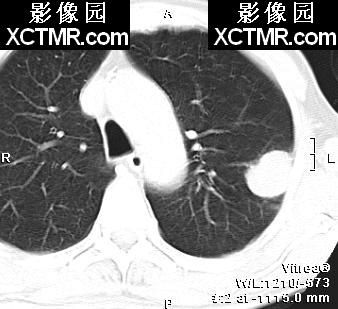
此病例肺结节表现“小泡征”、“胸膜凹陷征”,手术病理证实为肺腺癌。
STS-MIP 肺结节检查的CT检查方法众多,包括:簿层扫描、HRCT扫描、螺旋扫描、动态增强扫描、双能CT扫描、双气相同层面对比扫描以及各种后处理技术等,我们特别推荐靶螺旋扫描――一种窄准直与小FOV相结合的扫描技术。技术参数:小FOV(包括纵隔和一侧肺,20-25cm),扫描层厚约为结节直径的1/3~1/2,根据结节大小而定,取2~5mm,p=1~2,重叠40%~100%重建。若FOV小于20cm,则噪声等的增加将使分辨力不能进一步提高,甚至会降低;若FOV太大,则分辨力下降,将失去靶的意义。 靶扫描一方面提高了分辨力,另一方面有助于详细的密度分析,在靶扫描的基础上,可以更好地完成上述各种扫描,尤其建立时间-密度曲线,同时还可以结合选择性血管造影进行CTBA和CTPA的研究。缺点是覆盖范围较小,常需与常规扫描同时使用。
靶扫描与“靶重建”不同,后者在常规螺旋CT数据的基础上缩小FOV、并重叠重建,虽然图像较常规要好,但较常规螺旋CT并不增加信息,其优点是不需再扫描,对较大而典型的结节应用较好;对小结节或疑难结节仍以靶扫描为佳。视窗的调节是一个看似简单却很重要的小环节,临床实际使用中五花八门。由于不同的机型和照相机工作状态不同,视窗有所不同;对于一个可疑的肺内小病灶,不适当的视窗会导致误漏诊或延诊。总结我们多年的使用经验,有这样一个原则:病灶的多成分性决定了单一视窗常不能满足需要,要以待显示病灶的密度为轴心进行调整,作多视窗显示。具体做法为:①常规肺窗要求既有层次,又有对比,一方面要有一定的窗宽,我们通常用1000~1200HU,另一方面将窗中心调至-450~-500HU,可兼顾到大多数病变的显示;②浅淡的病变如磨玻璃影、粟粒结节,密度低于结节,用常规视窗有时不太清楚,需将窗宽及窗中心均作下调;
③显示空泡征或支气管充气征时,窗宽应稍宽,太窄的窗宽因图像太白而可能掩盖低密度的空泡及支气管;
④结节密度测定时,用纵隔窗,窗宽设为350HU左右,窗中心设定以结节平均密度为佳,常为45~60HU;
⑤其它特殊情况特殊处理。
对于一个周围性肺结节,特征显示包括三方面:形态学特征、结节-肺界面和邻近改变;血管改变贯穿以上三方面。
一、形态学特征――直接而根本的征像,显示原则是“多层面、多方位”
1.形态(morphology)
①圆形肿块征,表现为病灶趋圆形(类圆形),体现了其生长方式为细胞的堆积,以与三角形、长条形及片状病灶区分。技术上以后处理3D-SSD为佳,能立体、直接而有效地作出评价,MPR也有很好的价值,而常规横断面评价时要有一定的经验,在脑中“重组”病灶立体形象。
②分叶征(lobulation),是指肿块的轮廓并非纯粹的圆形或椭圆形,表面常呈凹凸不平的多个弧形,形似多个结节融合而成,通常可分为深分叶和浅分叶,以分叶部分的弧度为标准:弦距与距长之比>2/5为深分叶。病理基础一是与肿瘤边缘各部位肿瘤细胞分化程度不一,生长速度不同有关。二是肺的结缔组织间隔,进入肿瘤的血管、支气管分支、从肿瘤内向外生长的血管和结缔组织等可引起肿瘤生长受限,产生凹陷,从而形成分叶的形态。深分叶征在肺癌诊断中有重要意义。技术上以靶扫描为佳,重叠重建常有必要,结合横断面和非横断二维图像可以有效区分,3D重建则可提供直观但并不很精确的图像。 ③棘状突起(spiculate protuberance),含义与毛刺不一样,病理上有肿瘤的直接侵犯,影像上指介于分叶与毛刺之间的一种较粗大而钝的结构,有时也称为一种特殊的分叶,
许多研究认为,棘状突起只见于肺癌,因而,其检出的重要性可见一斑,但难点是准确认识;靶扫描能够很好地显示肿块边缘及棘状突起,而3D也能较好地显示这种“杵状”结构。 ④结节征(nodule sign)与⑤空泡征(vocule sign),前者指病灶内呈多个圆形结节样,即由多个结节组成,见于早期肺癌,其病理基础是肺癌的多灶性起源,尚未融合;后者指病灶内1-2mm(或<5mm)的点状透亮影,单个或多个,也主要见于早期肺癌,其病理基础主要是尚未被肿瘤破坏、替代的肺结构支架如肺泡、扩展扭曲的未闭细支气管等,部分是肿瘤坏死腔、含粘液的腺腔结构。这两个征像常共存,只能在薄层扫描图像能够较好显示,通常以HRCT显示,但常因不是容积扫描而未能在准确位置;靶扫描因为有重叠重建、重置中心则显示更佳;其技术关键在于薄层。
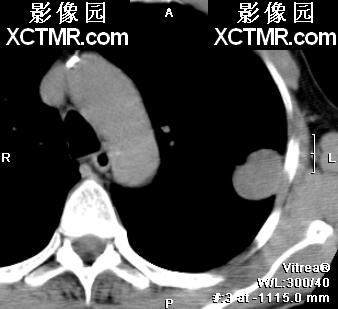
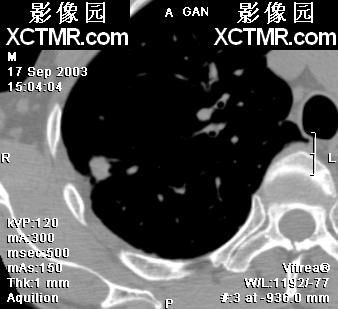
此病例肺结节见分叶征,手术病理证实是肺鳞癌。
⑥空洞征,指病灶内较大而无管状形态的透亮影,病理上指结节内有坏死液化并排出所致。影像上定义为大于相应支气管经2倍、且与上下层面支气管不连续的灶内透亮影,或大于5mm的圆形或类圆形空气样低密度影,有多种形态,包括薄壁/厚壁空洞、中央性/偏心性空洞、壁光整或不规则、有无壁结节等。肿瘤空洞多为中央性厚壁空洞,壁不规则,可有壁结节。壁厚度≤4mm倾向于良性,≥15mm倾向于恶性。同上述征像,该征也以薄层或靶扫描显示为佳。
2.密度(density) 密度是用以评价肺结节内部组织特性的重要参数之一。密度评价包括平扫密度和增强后密度变化,其中一种热门而又较好的分法是建立TDC(线图),日常工作中最少可用三个时间点替代:增强前、增强后早期(30-40s)、延迟(约4-5min)。密度测定的技术要求:
①使用区域值(ROI),区域象素不少于最小值,如前所述对于均匀结节采用60%面积或直径取ROI,或者尽可能包括整个结节但避免边缘有部分容积效应的部分;
②分区测定,对于不均匀的结节,应对不同密度区域分别测定和评价,避免互相影响; ③应避开钙化、坏死及空洞等。
动态增强的研究近年较为热门,Swensen等的研究结果是恶性肿瘤组强化值(平均40Hu)明显高于良性组(平均11Hu),并认为以20Hu为阈值可有效鉴别良恶性结节,Yama等的结果相似;国内也有不少研究,将结节分为三类,并提出强化值≤20Hu高度提示良性,20-60Hu提示恶性,>60Hu以炎性结节可能大,我们的结果与此一致。研究还表明结节强化程度与直径无关。近年,增强研究从全结节深入到结节区域性评价,对结节各部分分别测定密度值,然后综合分析,以期提高诊断准确率。从肺密度方面、依据肺窗→纵隔
窗转换时病变最大层面面积减少的比率(作者称为“肺纵隔窗缩减率”)将肺小结节分三型,致密型:缩减率小于50%,病变大小无明显变化;含气型:缩减率100%,纵隔窗上病变完全消失;中间型:缩减率大于50%,介于两者之间。这不失为一种实用手段,尤其适用于基层。
完成密度分析的技术以靶扫描为最佳。层厚较小,结构显示详细,密度值越有价值,但层厚过小则所含象素体积太小而影响密度值的代表性,故应适当取值,通常以结节直径的1/3作层厚为佳。螺旋扫描可以达到同样效果,且最易完成经病灶中央的扫描,因而最具临床应用价值。HRCT使用高分辨力或称高频算法,增加了噪声,出现边缘增强效应,高估了象素信息;soft算法正相反,低估了象素信息,只有标准算法即没有信息的增加,也没有信息的减少,接近结节的本来面目,适合密度测定。3.钙化,calcification 明显的钙化在普通CT上即可辨认,但细微的钙化常常遗漏。国外作者将钙化定义为CT值大于164HU的结构,以此为标准的阳性率低,因而国内有作者将阈值修正为100HU,但据我们的经验,阳性率仍然偏低。而钙化对小结节的定性具有重要作用,因而有必要作详细的进一步显示。
①簿层扫描:一方面提高了分辨力(高组织对比度下的空间分辨力),另一方面减少了部分容积效应,增加了密度对比,明显提高钙化检出,结合小FOV则更佳。螺旋CT是实现这一方法的最佳技术。
②HRCT:不少作者认为这是一种显示钙化及内部结构的良好技术,一般地,该技术对检出结节内部的钙化不错,但由于高分辨力算法的边缘增强效应,容易产生假像,增加钙化的假阳性率,因而要慎重使用。
③双能CT扫描:Bhalla等[6]报道27 例双能CT扫描:11例密度升高的结节中良性10例;李云卿等报道15例扫描:9例密度升高的结节中良性8例,6例密度降低的结节中恶性4例。Swensen等 的多中心研究则否定了这种技术。
④phantom CT:国外有作者[15]提出利用视窗技术,调整窗宽1-2HU、窗中心164HU,凡可密度在164HU以上的均可显示,提示良性结节。据我们的经验,窗中心可根据需要设定不同值,因为平扫平均密度在60HU以上的小结节很少有恶性的,这样可提高敏感性。 钙化的分布、形态、及含量也很重要。Mahoney等分析395例发现:稠密、中心、层状、爆米花样及散在的钙化多为良性,而点状、网状、不定形的钙化多为恶性;李云卿等发现8例密度升高的良性结节,其钙化分布为稠密、中心或散在,1例鳞癌为点状钙化。
4.支气管征,bronchus sign 上下层连续、长条或分支状、与支气管相关或血管伴行的小透亮影定义为支气管气相(air bronchogram, AB征) 。这种结节内支气管影在不同的病理条件下表现不同,有研究者提出对这种支气管的形态进行分析有助于定性诊断。良性病变中的支气管结构完整、没有破坏,其内壁光滑,因而管腔多为正常形态。恶性病变中的支气管一方面受到侵犯,导致管腔狭窄、截断、内壁不光、管壁增厚僵硬等;另一方面,肿瘤常有粘稠分泌物,可导致支气管扩张,远端粗于近端,这种支气管扩张虽也可见于良性病变,但少见,至于支气管的外压性改变则无定性意义。 对结节内透亮影难以确定是空泡征、空洞征还是支气管气相时,不妨采用纯粹的形态学分型。古谷清美等将结节内透亮影分为管型(呈细长管状或连续多层面小圆形影)、囊型(类圆形或多形态的囊状),分析163例SPN中有透亮影的60例(肺癌41,转移2,结核4,炎症13)发现:管型45=肺癌31+炎症与结核14,多为1-2个管型;囊型33=肺癌29+炎症4,多囊(≥3个)22均为肺癌(包括2例转移)。作者认为多囊透亮影提示恶性倾向。显示结节内支气管
征的技术关键仍是薄层扫描,连续图像显示也很关键,因而以靶扫描为佳,有时也用HRCT,但常缺乏上下层面的相关分析;若同时结合增强扫描有时更有帮助;后处理如MPR重建有助于显示斜行的支气管征,但由于分辨力的关系,其实际意义并不大,最新的Multi CT所能达到的各向同性成像理论上看可有帮助。
二、结节-肺界面(或称界面征,interface sign) 界面征主要有:
边缘清楚――即结节轮廓与含气的肺实质对比分明,轮廓清晰可辨,可锐利或有毛刺。光滑锐利――结节与肺实质之间清晰、截然,如笔画一样。毛刺征――表现为自结节边缘向周围伸展的、放射状的、无分支的、直而有力的细短线条影,近结节端略粗;同义词有毛刷征,典型者也称放射冠。部分结节可见周围环绕的气肿带,晕轮状,衬托出明显的毛刺样改变。部分毛刺较长,也称长毛刺。
尖角征、桃尖征――通常数量较少,表现为较粗大而长的线条影,近端更粗大,呈明显的尖的突起状,其远端常可有长线条牵引,主要与棘状突起鉴别。
索条征――表现为粗长而不规则的线条影,常有分支。
模糊征――表现为结节轮廓欠清,边缘难以确定;肺窗上可见而纵隔窗上消失。充血征――结节周边向周围伸展的、模糊的、软而无力的略弯曲线条影,可有分支。主要与毛刺鉴别。 这是一种形态学的显示,通常在普通CT上即可显示,无需增强,但较粗糙。该界面对比度大,因而用高空间频率算法重建的图像对此显示佳。我们的工作中发现HRCT显示界面最佳,但常只能单层显示,做不到容积成像;螺旋靶扫描有相当接近的分辨力,且为容积成像,可以更详细显示界面,综合判断力更佳,尤其同时可以考虑其它情况,较为实用。有时也直接从螺旋CT扫描数据中进行高频率算法重建,虽质量不如HRCT,但也能较好达到目的;或进行螺旋HRCT扫描成像。 传统上无需增强扫描了解界面,但为了分析界面范围的血管征,可作增强扫描分析。1.胸膜凹陷征(pleural indentation)与胸膜反应(pleural reaction)―― 胸膜凹陷征的病理基础主要有两个方面:一是结节内纤维瘢痕收缩牵拉,二是胸膜没有增厚、粘连;表现为规则线条影自结节牵拉胸膜,胸膜凹入形成典型喇叭口状,胸膜凹入处为液体,但连接于叶间裂时仅见叶间裂凹入而无液体积聚。胸膜反应的病理基础包括炎性纤维化性反应或肿瘤性侵犯,导致胸膜增厚、粘连,尽管也有条状连接影,但没有胸膜凹入。CT上,胸膜凹陷征主要有三种表现:
①当凹入中心与扫描层面平行时显示出典型的胸膜凹陷征──瘤灶与邻近胸壁间三角形影或称喇叭口,其尖端与线状影相切;
②当扫描层面偏离凹陷中心时,线状影由1条分为两条或两条以上,有时见其与瘤体逐渐分开,三角形影由大变小,分成两个小三角形;
③水平裂和斜裂胸处表现为曲线影。 充分显示胸膜凹入处的液体及无增厚的胸膜是诊断关键,薄层扫描尤其靶螺旋CT可以准确显示。一些作者采用HRCT分析,也取得了较好的效果;3D重建可以直观、详细地显示胸膜凹陷征的情况。2.血管征 结节的血管征有肺血管包被征、血管集束征、周围血管充血征及单纯血管推移征。也有作者将SPN与周围血管的关系分为四种:血管穿过结节、血管向结节移位、血管在结节周边截断、血管受压移位;
1)肺血管包被征――指肺血管进入结节或终止于结节,血管常狭窄、堵塞、截断等,文献认为其中以肺静脉包被(肺静脉包被征)意义最大,提示肺癌机会增加。2)周围血管充血征――指前述的界面征中的充血征。
3)血管集束征――指邻近血管向结节聚拢,常可见多根细小血管向结节聚集。其本质仍是病灶内纤维增生,牵拉邻近肺结构包括血管,形成可见的血管分布改变。有作者认为此种改变主要见于穿越肺间隔的静脉。Yang等做血管造影-病理相关性研究后认为:结节边缘的血管聚集为病灶内疤痕所致,也是结核瘤毛刺征的病理基础,血管聚集征和肿块远侧血管扩张征并非为周围型小肺癌所特有,在肺癌与结核瘤中出现率相似。4)单纯血管推移征――血管受结节推挤而改变走向。
关于血管征的确认、病理及其意义均有不同的看法,国内外不少作者认为肺静脉包被、聚集可能更多地见于恶性病变。根据我们的经验,这种倾向性并不明显,然而,只要是较明显的稍粗大的血管聚拢于结节,对肺癌的诊断仍有一定的帮助。国内也有报道血管集中征有助于肺癌的诊断。
3.显示技术同前述的支气管血管束征。
卫星病灶――卫星病灶通常较小、密度较低,边缘可清楚或模糊,甚至呈斑片状,薄层扫描可较好显示;螺旋靶扫描则显示极佳,适当的窗位可能较为重要。
第二篇:CT肺结节


Managing the Small Pulmonary NoduleDiscovered by CT*
Daniel M. Libby, James P. Smith, Nasser K. Altorki, Mark W. Pasmantier,David Yankelevitz and Claudia I. Henschke Chest 2004;125;1522-1529DOI 10.1378/chest.125.4.1522 The online version of this article, along with updated informationand services can be found online on the World Wide Web at: /content/125/4/1522.full.html
CHEST is the official journal of the American College of ChestPhysicians. It has been published monthly since 1935. Copyright

2004by the American College of Chest Physicians, 3300 Dundee Road, Northbrook, IL 60062. All rights reserved. No part of this article or PDFmay be reproduced or distributed without the prior written permission of the copyright holder.(/site/misc/reprints.xhtml)ISSN:0012-3692
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
opinions/hypotheses
ManagingtheSmallPulmonaryNodule
DiscoveredbyCT*
DanielM.Libby,MD,FCCP;JamesP.Smith,MD,FCCP;NasserK.Altorki,MD,FCCP;MarkW.Pasmantier,MD;DavidYankelevitz,MD;andClaudiaI.Henschke,PhD,MDObjectives:ToreviewtheEarlyLungCancerActionProjectexperienceandthemedicalliteraturefrom1993to2003ondetectionofthesmall,noncalcifiedpulmonarynodulebyCTinordertoformulateamanagementalgorithmforthesenodules.
Design:ProspectivenoncomparativestudyofsmokerswithoutpriormalignancyandareviewofthemedicalliteratureofCTscreeningoflungcancer.
Interventions:ChestCTand,whereappropriate,CTobservationfornodulegrowth,antibiotics,CT-guidedfine-needleaspiration(FNA)biopsy,fiberopticbronchoscopy,andvideo-assistedthoracoscopicsurgery(VATS).
Results:ThefollowingfactorsinfluencetheprobabilityofmalignancyinaCT-detected,small,noncalcifiedpulmonarynodule:size,changeinsize,age,smokinghistory,density,numberofnodules,gender,circumstanceoftheCT,spirometry,occupationalhistory,andendemicgranulomatousdisease.ThetwodiagnostictechniquesmostusefulinevaluatingtheCT-detected,small,noncalcifiednoduleareshort-termobservationofnodulegrowthbyCTandCT-guidedFNA.Duetosmallnodulesizeandthefrequentfindingofnonsolidorpart-solidnodules,positronemissiontomography,fiberopticbronchoscopy,andVATSwerelessuseful.
Conclusions:PulmonologistsarefrequentlyaskedtoevaluatetheCT-detected,small,noncalci-fiednoduleinvisibleonstandardchestradiography.Immediatebiopsyisjustifiedifthelikelihoodofcancerishigh,butifthatlikelihoodisloworintermediate,aperiodofobservationbyCTisappropriate.VATSorthoracotomyarerarelynecessaryforadiagnosisoflungcancerintheCT-detectedsmallpulmonarynodule.(CHEST2004;125:1522–1529)Keywords:CT-detectedpulmonarynodule;earlylungcancerdetection;management
Abbreviations:CXR?chestradiography;ELCAP?EarlyLungCancerActionProject;FNA?fine-needleaspira-
tion;PET?positronemissiontomography;3D?threedimensional;VATS?video-assistedthoracoscopicsurgery
lungcancerisnotthemostcommonAlthough
typeofcancer,itistheleadingcauseofcancer
deathintheUnitedStates.1Thismayresultfrom
*FromtheDepartmentofMedicine(Drs.LibbyandSmith),
DivisionofPulmonaryandCriticalCareMedicine;DepartmentofSurgery(Dr.Altorki),DivisionofCardiothoracicSurgery;DepartmentofMedicine(Dr.Pasmantier),DivisionofHema-tology-Oncology;andDepartmentofRadiology(Drs.YankelevitzandHenschke),DivisionofThoracicRadiology,WeillMedicalCollegeofCornellUniversity,NewYork,NY.ManuscriptreceivedMay9,2003;revisionacceptedOctober16,2003.Reproductionofthisarticleisprohibitedwithoutwrittenpermis-sionfromtheAmericanCollegeofChestPhysicians(e-mail:permissions@chestnet.org).Correspondenceto:DanielM.Libby,MD,FCCP,407EastSeventiethSt,NewYork,NY10021
1522intrinsicaggressivebiologicalbehavior,latediagnosisand,untilrecently,littleattentiontoscreeningforlungcancer.Aswithotherepithelialcancers,thereislikelyawiderangeofbiologicalbehaviorsintrinsictolungcancer.Inpatientswhoselungcancerisde-tectedinstageI,thecurerateis70%.2However,trialstodetermineifscreeningreducedlungcancermortalityinthe1970sand1980s,utilizingthebesttechnologyoftheday,chestradiography(CXR),andsputumcytology,didnotdemonstrateadecreaseinlungcancermortality,perhapsbecauseonly30%oflungcancersdiscoveredwithCXRscreeningwereinstageI.3–6Fewerthan10%ofpatientswhoselungcancerwasdiscoveredbythedevelopmentofsymp-toms(noscreening)werestageI.4Overthepast10Opinions/Hypotheses
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
years,lungcancerscreeningstudiesusingCThavedetectedupto85%oflungcancersinstageI,offeringpromiseinwhathasbeenadiseasewithadismaloutlook.7–14
Physiciansarethereforeincreasinglyaskedtodi-agnose,manage,andtreatever-smallerpulmonarynodulesdiscoveredonCTperformedeitherforlungcancerdetection,coronaryarterydiseasescreening,orforotherreasons.ThisisareviewoftheprinciplesofdiagnosisandmanagementofsmallpulmonarynodulesgainedthroughourexperienceinpatientswiththeEarlyLungCancerActionProject(ELCAP)andthesubsequentprojects(NewYorkELCAPandInternationalELCAP).15,16
MaterialsandMethods
WereviewedourexperiencewithlungcancerscreeningbyCT
inpatientswithoutpriormalignancyattheWeillMedicalCollege
ofCornellUniversityELCAPfrom1993tothepresent,and
performedareviewoftheliteratureusingMEDLINEtoevalu-
ateallpublishedstudiesofCTscreeningforlungcancerto
determinethebestapproachtothediagnosisandmanagementof
thesmallpulmonarynodule.Asmallpulmonarynodulewas
definedasanopacityinthepulmonaryparenchyma?3cmin
greatestdimensionwithadensitygreaterthanthesurrounding
lungtissue.Theresultinganalysiswasorganizedintotwosec-
tions:factorsinfluencingtheprobabilityoflungcancerina
pulmonarynodule,andtechniquesutilizedinthediagnosisofthe
smallpulmonarynoduledetectedbyCT.size.Lungcancerappearstoberareinnodules?5mminsize,anditissafetorepeattheCTat1yearinthesepatients(Fig1,top).7,8Theimportanceofsizeindeterminingthelikelihoodoflungcancerinapulmonarynoduleisinfluencedbytheageofthesubjectandthecircumstanceofthestudy.Forexample,inELCAP,asweloweredtheminimumageforlungcancerscreeningfrom60to40years,wefoundlungcancerincidenceinnodules?15mmindiameteronbaselinescreeningtobeaslowas5%.Thus,immediatebiopsyisnolongerrecommendedfornodules?15mmfoundonbaselinescreening.Aperiodofradiographicobservationforgrowth(withorwithoutantibiotics,dependingontheclinicalcircumstances)isappropriate(Fig1,top).19Newnodulesdiscoveredona1-yearrepeatCTmorefrequentlycontaincancerandatsmallersizethanonthebaselineCT.7,8ChangeinSize:Anodulethatincreasesinsizeisassumedtobeactive;ifitdoublesinvolumein?1month,itsgrowthrateisuncharacteristicoflungcancer.Anodulethatgrowsatarateconsistentwithcancer(doublingtimeof30to360days)shouldbesampledforbiopsyorresected,20althoughslower-growinglungcancershavebeendescribed.ItisimportanttorememberthatCToffersatwo-dimen-sionalview,unlessthree-dimensional(3D)softwareisavailable.Ifsuchsoftwareisnotavailable,esti-matesofnodulegrowthmustrelyondiameterratherthandirectmeasurementofvolumeinassessmentofdoublingtime,whichislessaccurate.
NumberofNodules:IntheinitialELCAPreport,apositivefindingwasdefinedasonetosixnoncal-cifiedpulmonarynodules;morethansixnoduleswerethoughttoindicateinflammatorylungdisease,andthishasbeenconfirmedafteryearsoffollow-up.7SynchronouslungcancersareincreasinglyrecognizedasCTscreeninghasbecomemoreprev-alent,andmultifocalbronchoalveolarcelloradeno-carcinomaisoftenthehistology,particularlyinwomenwhoneversmokedorquitcigarettesmokingmanyyearsearlier.Wefollowupanynewnoduleonrepeatscreeningandallnodules?5mmonbaseline.
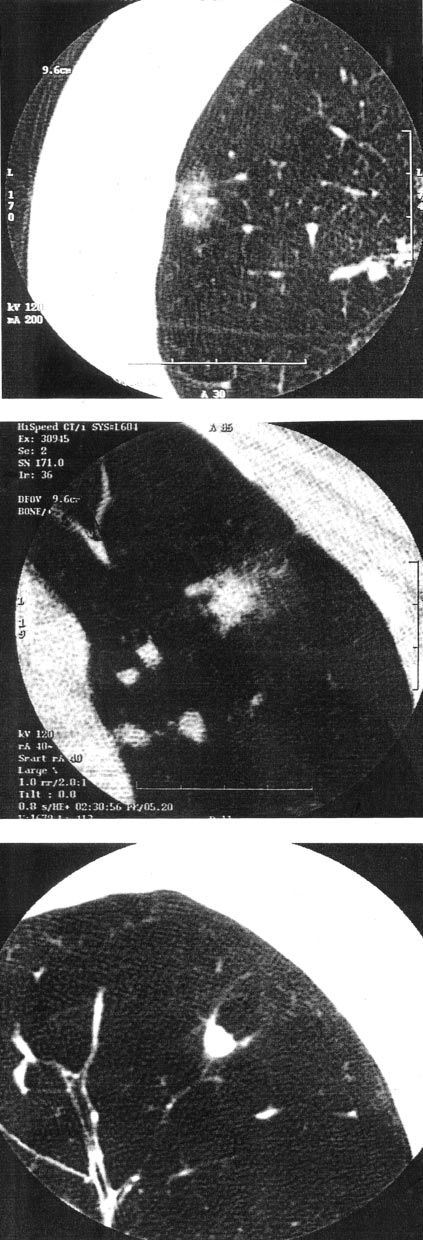
Density:WhileCXRonlypermitsidentificationofsolidnodules,theuseofCTledtoincreasingrecognitionofsubsolid(nonsolidandpart-solid)nodules(Fig2).21Anonsolidnodule(previouslytermedground-glassopacity)isadensitythroughwhichaeratedlungparenchymaisvisible.Apart-solidnodulecontainsasolidcomponentthatoblit-eratestheaeratedlungandalsocontainsanonsolid
CHEST/125/4/APRIL,2004ResultsFactorsInfluencingtheProbabilityofLungCancerinaPulmonaryNoduleSize:SinceCXRstudieshaveshownthelikelihoodofcancerinsolitarypulmonarynodules,ithasbeenrecognizedthatnodulesizecorrelateswiththeriskofcancer,17butuntilCTtherewerelittledataonnodules?1.5to2.0cmindiameter(Table1).18ItisdifficulttorecognizelungcancerbyCTinnodules?5mmindiameteramongthemanynodulesofthisTable1—FactorsInfluencingtheProbabilityofCancerinaPulmonaryNoduleSizeChangeinsize(growth)NumberDensityCircumstanceofCTPatientageGenderCigarettesmokinghistorySpirometryOccupationalhistoryE1523
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
component.Nonsolidnodulespossessarelativelylowriskofcancer(approximately15%);astheirsizerises?1.5cm,theriskofmalignancy,particularlyadenocarcinomawithbronchoalveolarcellfeatures,rises.Part-solidnodulesarethemostlikelyofnod-ules?1.5cmindiametertocontainlungcancer(approximately40to50%),andtheriskofcancerrisesasthesizeofthenodule,particularlythesolidcomponent,increases.21Althoughsolidnodulesarethemostcommon,alowerproportionarecancer.Inflammatorydiseasesofthelung,particularlytu-berculosis(typicalandatypical)andmycoses,gener-allyproducesolidnodulesthatcanbeexpectedtoeventuallycalcify,permittingtheirdesignationasbenign.Onlyapproximately15%ofsolidnodules?1indiametercontaincancer,butassolidnodulesizeincreases,theproportionthatiscancerin-creases.Despitethelowerproportionofsolidnod-ulesthatarecancer,becausetherearemanymoresolidthansubsolidnodules,mostlungcancersarefoundinsolidnodules.Thereappearstobeaprogressionfromnonsolidtopart-solidtosolidnod-ule.Thenonsolidnodulemayrepresent,insomeinstances,inflammatorydisease;inothers,itmaycontainpremalignantlesionssuchasatypicaladeno-matoushyperplasiaorbronchoalveolarhyperplasia.22
Thenonsolidnodulemayalsorepresentbronchoal-veolarcarcinomaorinvasiveadenocarcinomawithbronchoalveolarcellfeatures.Noguchietal23de-visedahistopathologicclassification(typesAtoD)describingprogressivelygreatermalignantpotentialandpropensitytolocoregionalmetastases.Thepart-solidlesionoftencontainsinvasiveadenocarcinomainthesolidcomponent.Solidnodulescontainingcancermaycontainadenocarcinomaorothercelltypessuchasepidermoid,large-cellanaplastic,neu-roendocrine,carcinoid(typicaloratypical)or,leastlikely,small-cellcarcinoma.
CircumstanceoftheCTStudy:IfchestCTisperformedtoscreenforlungcancer,theinitialbaselinestudymaycontainnodulesresultingfrompriorinflammatorydisordersorlungcancer.IntheELCAPseriesof1,000subjectsundergoingtheinitialbaselinescreenCT,233subjects(23.3%)hadonetosixnoncalcifiedpulmonarynodules.7How-ever,thenumberofnewnodulesdiscoveredontherepeatscreeningstudyayearlaterwasonly30(2.5%of1,184repeatscreenings).8Foranewnodulediscoveredonthe1-yearintervalscreeningstudy,acourseofantibioticshasbeensuggested(witharepeatdiagnosticCT4to6weekslater);indeed,itwasfoundthatin12ofthe30patients,thenewrepeatscreenCT-diagnosednodulesresolved4to6weekslater.8Ofthe18patientswithnewpersistentnodulesonthe1-yearintervalscreeningstudy,
7
Opinions/HypothesesFigure1.Top:Prebiopsyalgorithmformanagement.Bottom:Postbiopsyalgorithmformanagement.1524
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
subjects(39%)hadlungcancer,amuchhigherproportionthanwasfoundatbaseline(27of233subjects[12%]).Thus,abaselinescreeningCTismuchmorelikelytohaveafalse-positiveresultthanthe1-yearintervalscreeningstudy.ChestCTper-formedincidentallyinanindividualwithoutrespira-torysignsorsymptomsprobablypossessesthesamechanceofcontainingapulmonarynoduleasabase-linescreeningstudy(23%);giventhesameriskprofileofageandsmokinghistory,thenodulesdiscoveredwouldcontainthesameproportionoflungcancersasabaselinescreeningstudy(12%).
Age:Lungcancerisrarebeforetheageof40years,butitsincidenceincreasessteadilyfrom40to80years.1Thisdepends,however,ontheagewhensmokingstarted.Afterage80years,theincidenceoflungcancerlevelsoffandmaydecline.StudiesofCTscreeningforlungcancerfromJapan9,10,12,13thatincludedpatientsaged?40yearshadamuchlowerincidenceofcancerinpulmonarynodulesthandidscreeningstudies7,8fromtheUnitedStatesthatincludedpatients?60yearsold.
Gender:Ascigarettesmokinghasincreasedinwomen,theincidenceoflungcancerhasrisen.24
Womenmaybeathigherriskthanequallysmokingmenofthesameage,perhapsrelatedtogeneticallylinkeddifferencesinenzymesinvolvedinthedetox-ificationofcarcinogensincigarettesmoke.
CigaretteSmokingHistory:Theincidenceoflungcancerdirectlycorrelateswiththepack-yearsofcigarettessmoked.25Whileithadbeenthoughtthatsmokingcessationproducedaprogressivedropinlungcancerincidence,thisconcepthasbeenques-tioned.26Itappearsthattheincidenceoflungcancerstopsincreasingaftersmokingcessation,butitdoesnotdroptothelevelsofindividualswhoneversmoked.Consequently,itiscommontoencounterpatientswithnewlydiagnosedlungcancerwhostoppedsmokingmanyyearsordecadesearlier.ThechangeinsmokinghabitsintheUnitedStatestowardlow-tarandfiltercigaretteshasinfluencedtheclin-icalpresentationoflungcancer.Changingsmokinghabitsareassociatedwiththeriseofadenocarcinomatothemostcommonhistologicsubtype.27Small-cellcarcinoma,thecelltypemostcloselyassociatedwithcigarettesmoking,hasbecometheleastcommonhistology.Thelocationoftheprimarytumorhasmirroredthesechangesinhistologyandsmokinghabits,forperipheraladenocarcinomashavebecomemuchmorecommonthanlargeairwaylesions.Itisthoughtthatsmokersoflow-tar,filtercigarettesinhalemoredeeplyandretainsmokeinmore
pe-
CHEST/125/4/APRIL,2004Figure2.DensityofpulmonarynodulesseenonCT.Top:Nonsolidnodule;aeratedlungparenchymaisvisiblewithinthenodule.Middle:Part-solidnodule,whichcontainsasolidcom-ponentandanonsolidcomponent.Bottom:Solidnodule.1525
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
ripheralportionsofthelung(andthusacquireperipheraladenocarcinomas)thandosmokersofnonfilter,high-tarcigarettes(whoacquirecentralairwaylesionsofothercelltypes).ItisfortuitousthatCThascomeintocommonuseconcurrentlywiththischangeinsmokinghabitsintheUnitedStates,sinceitismoreaccurateindetectingperipherallungcancers.Lungcancerscreeningstudiesthatincludesmokersandnonsmokerswouldbeexpectedtoshowalowerincidenceofcancerinpulmonarynodulesthanstudiesthatrequireentrantstohavesmoked10to20pack-years,thusexplainingthedifferentpro-portionsofpatientswithcancerinpulmonarynod-ulesreportedfromJapan,theUnitedStates,andEurope.7–14
SpirometricFindings:Thereisastatisticallysig-nificantassociationbetweenaspirometricallydem-onstratedobstructiveventilatoryimpairmentandlungcancer.28Aftercontrollingforthenumberofcigarettessmoked,smokerswithreducedFEV1/FVCratioshaveahigherriskofacquiringlungcancer,particularlylungcancerinvolvinglargeairways,thansmokerswithoutanobstructiveventilatoryimpair-ment.Thishasledtotherecommendationthatthespirometricfindingofanobstructiveventilatoryim-pairmentshouldbepresentwithequalfrequency(stratification)instudiescomparingscreeningwithnoscreeningandinlungcancerpreventionstudies.Inordertostudythehighestriskgrouppossible(andtherebylimitthefalse-positiverateofthescreeningtest),someinvestigatorshaveincluded,alongwithageandsmokinghistory,anFEV1/FVCof?0.7asanentrycriteria.11Althoughthisprovidesforahigherriskgroup,itbiasesthesestudiestowardincludingahigherpercentagesofpatientswithlargeairwaycancers.
OccupationalHistory:Asbestosexposure,afteralatencyperiodof20to40years,predisposestolungcanceractingsynergisticallywiththeriskposedbycigarettesmoking.Workersexposedtorespirableradioactivegasintheproductionanddisposaloffissionablematerialshaveanincreasedriskoflungcancer,althoughtheriskhasnotbeenaswellquantifiedastheasbestosrisk.29InternationalELCAPiscurrentlystudyingthisgroupwithCT.Uraniumminersandindividualsworkingwithheavymetalssuchascadmiumandnickelareknowntohaveanincreasedlungcancerrisk.Individualswithidiopathicpulmonaryfibrosisandpneumoconiosesprobablyhaveanincreasedriskofacquiringadeno-carcinomaorbronchoalveolarcellcarcinoma.30
EndemicGranulomatousDisease:InstudiesofCXRscreeningforlungcancerinthe1950sand
15261960s,mostlungnoduleswereduetoMycobacte-riumtuberculosis.Asthenationwideincidenceoftuberculosishasdeclined,exceptnotablyinimmi-grantsfromendemicareasandinHIV-positiveindividuals,Mtuberculosishasbecomealesscom-monetiologyofpulmonarynodules.WhenCTscreeningforlungcancerwasperformedintheMidwestUnitedStates,anareaendemicwithhis-toplasmosis,ahighfalse-positiveratewasob-served.11Similarly,instudiescurrentlyunderwayinChina,ahigherfalse-positiveratewillbeanexpectedfindingduetothehighincidenceoftuberculosis.Atypicalmycobacterialinfection,usuallyduetoMy-cobacteriumaviumintracellulareorMycobacteriumkansasii,hasbeenobservedinapparentlyhealthypeople,olderwomeninparticular,andisoftenassociatedwithperipheralbronchiectasisandmu-coidimpaction.DiagnosticTechniquesforManagingtheSmallPulmonaryNoduleDetectedbyCTCTAssessmentofNoduleGrowth:AssessmentofnodulegrowthbyCThasbecomesuchanimportantpredictiveparameter,withorwithouttheuseof3Dsoftware,thatitmaycircumventtheneedforotherdiagnostictechniques(seebelow).Anodule?5mmindiameteroranonsolidnodule5to9mmindiameterpossessaverylowriskofmalignancy,soELCAPrecommendsarepeatCTin1year(Table2).Part-solidorsolidnodules5to9mminsizeandsomenodules?10mminsizehaveanintermediatelikelihoodofmalignancy;therefore,arepeatCTin6weekstoassessfornodulegrowthorresolution(withorwithoutantibiotics)maybeuseful(Fig1,top).FurtherCTassessmentfornodulegrowthafter3monthsisreasonableforthosenodulesthatare“nonspecificbenign”onfine-needleaspiration(FNA)andforthosenodulesthatpartiallyresolveordonotchangeafterantibioticsonthe6-weekCT.Ifdoublingtimes(estimatedbyconventionalCTor3Dsoftware)areintherangeof30to360days,biopsyorresectionmaybereasonableoptions.Ifanoduledoesnotgrowinvolumein6months,theriskofmalignancyisverysmall(?10%).Volumetricassess-mentofnodulesizemaypermitestimationofdou-blingtimeswithin6to12weekswhenchangeinsizeisnotapparentonstandardtwo-dimensionalCTTable2—Low-RiskNoncalcifiedPulmonaryNodulesDetectedbyCTNodulewithspecificbenigndiagnosisafterbiopsyPatientswithnodulesthathaveresolvedwithorwithoutantibioticsNodules?5mmindiameterNonsolidnodules5to9mmindiameterOpinions/Hypotheses
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
images.ThemedicalrisksofbiopsybyFNA,video-assistedthoracoscopicsurgery(VATS),orsurgery,andthefinancialexpenseofpositronemissionto-mography(PET)maybeavoidedbyrapidandaccurateassessmentofnodulegrowth.
PercutaneousFNABiopsy:FNAhasbeenusedinthediagnosisofpulmonarynodulesfor?25years(Fig1).FluoroscopicallyguidedFNAwaspopular-izedinSwedeninthe1970s.Biplanarfluoroscopyandtheintroductionofbiopsyneedlesprocuringacoreoftissueforhistopathologicevaluationwerefurtherrefinements.31WithCT,nodulesof5to15mmindiameterarefound,andCT-guidedFNAhasbecomeaveryimportantdiagnostictechnique,32
althoughitssensitivityandspecificityintheverysmallCT-detectednodules5to10mmindiameterneedverification.IninstitutionswhereCT-guidedFNAisnotperformed,therewilllikelybegreaterrelianceonCTassessmentofnodulegrowth.VATSandthoracotomywillprobablybeperformedforbenignnoduleswithsomewhatgreaterfrequencyifCT-guidedbiopsyofthesmall,noncalcifiednoduleisnotavailable.ThreetypesofresultsmaybeobtainedfromFNA:malignant,specificbenign,andnonspecificbenign.Thetreatmentimplicationsofamalignantdiagnosissuchascarcinomaorlymphomaareclear.Specificbenigndiagnosessuchastuberculosis(typicaloratypical),mycoses,nocardia,hamartoma,orbenignintrapulmonarylymphnodedonotrequiresurgeryandmaybemedicallytreatableorsafetoobserve.Anonspecificbenigndiagnosis,however,requirescarefulclinicalandradiographicfollow-up.Nonspe-cificbenigndiagnosesmightincludeatypicalbron-choalveolarhyperplasia,inflammation(granuloma-tousorother,withoutorganismsonsmearorculture),atypicalcells,etc.IffurthergrowthoccursafteranonspecificbenigndiagnosisisobtainedfromFNA,repeatbiopsyorresectionareindicated.
PET:PETusingfluorodeoxyglucoseisusefulinassessingthelikelihoodofmalignancyinapulmo-narynodule,particularlyifitissolidand?1cmindiameter.33False-positivePETfindingsinactivegranulomatousdiseaseandbenigntumorshavebeendescribed.Astandarduptakevalue?3issensitiveandspecificforcancer,butifthenoduleissubsolidor?1cmindiameter,sensitivityandspecificitydecline.34PEThaslimitedusefulnessinearlylungcancerdetectionwheremanynodulesare?1cmindiameterandmaybesubsolid.ThesensitivityofPETinadenocarcinomawithalveolarcellfeatureshasalsobeenquestioned.Onceadiagnosisoflungcancerhasbeenestablishedinasolidnodule,par-ticularlyifthereishighfluorodeoxyglucoseuptake,
PETmaybehelpfulindetectingmediastinallymphnodemetastasesevenwhenthenodesarenoten-largedonCT.34Clinicallyoccultextrathoracicme-tastasesorsynchronousextrathoracicprimarymalig-nanciesmaybediscoveredbyPET.FlexibleFiberopticBronchoscopy:Flexiblefiber-opticbronchoscopyhaslimitedusefulnessinthediagnosisofsmallperipheralnodules,35althoughtransbronchialneedleaspirationbiopsyincreasesthesensitivity.36Fiberopticbronchoscopyhasanimpor-tantroleintheuncommoncircumstanceofendo-bronchiallesionsdiscoveredonscreeningCT,anditcanbehelpfulindiagnosinginfectiousdiseasespresentingwithfocalpulmonarynodulessuchastuberculosis(typicaloratypical)ormycoses.VATS:VATSmaybeusefulinthediagnosisofperipheralpulmonarynoduleseludingdiagnosisbyothertechniques.Itismostaccurateinperipheral(within2cmofthepleura)solidlesions;nonsolidlesionsoftenproduceanormalappearanceonsur-gicalinspectionandmayprovedifficulttolocalizeduringVATS.DiscussionLungcanceriscommonand,underpresent“rou-tinecare,”commonlyfatal.InCXRscreening,lessthanonethirdoflungcancerswerediscoveredinstageI.Whilethisrepresentsagreatimprovementovernoscreening,itisnotsufficient.CTfindslungcancerinstageI85%ofthetime,afactdocumentedinmanythousandsofpatientsintheUnitedStates,Europe,andJapan.7–14Facedwithasmall,CT-detectedpulmonarynod-ule,thephysicianmustfirstassessthelikelihoodoflungcancer.Utilizingtheparametersofage,nodulesize,smokinghistory,spirometricfindings,occupa-tionalhistory,endemicgranulomatousdisease,thecircumstancesoftheCT(baselinescreen,interval1-yearscreen,orstudyperformedforotherreasons),thenumberofnodules,thepresenceofradiographicorclinicalsignsofinflammatorylungdiseasesuchasbronchiectasisoratypicaltuberculosis,andtheden-sityofthenodule(solid,nonsolid,orpartsolid),aninitialclinicalimpressionisformulated(Table1,Fig1).Iflungcancerishighlysuspectandthepatientisconsideredfitforthoracicsurgery,biopsyshouldbeundertaken.Ifthenoduleisjudgedtohaveanintermediatelikelihoodofbeinglungcancer,eitherPEToraperiodofradiographicobservationwitharepeatCTin6to12weeksshouldbesuggested.ForanoduleknowntobenewbyCT,aninfectiousetiologymaybepresent,andempiricantibioticsmayCHEST/125/4/APRIL,20041527
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
bejustified.WidespreaduseofantibioticsforCT-detected,smallpulmonarynodulesmaynotbeawisepractice,asitmayexacerbatetheproblemofantibioticresistance.Ifresolutionofthenoduleoccurs,nofurtherevaluationiswarranted;ifitgrows,biopsyshouldthenbedone.Ifnochangeoccurs,dependingonclinicalfactors,eitherbiopsyorfollow-upCTmaybereasonable.Ifanodulefailstochangeovera2-yearperiodonCT,itismostlikelybenign;ifitcontinuestogrowdespitebenignbiopsyfindings,particularlyifnonspecificbenign,itmuststillbeviewedwithsuspicionandeithersampledagainforbiopsyorresected.AstechnologicadvancesareappliedtoCT,particularlythewidespreadappli-cationofvolumetricanalysiscapableofestimatingdoublingtimesin6to8weeksandthedevelopmentofmultislicescannerscapableofproducingex-tremelythinslices,specificmanagementrecommen-dationsarelikelytochange.CytopathologicanalysisofFNAspecimensandhistopathologicstudyofresectedlesionshavechangedourconceptofthenaturalhistoryofsomelungcancers,andradiologic-pathologiccorrelationshaveemerged.Somelungcancersappeartobegininareasofbronchoalveolarhyperplasiaandsubse-quentlydevelopfeaturesofbronchoalveolarcarci-nomaand,finally,invasiveadenocarcinoma.37Thismaybeanalogoustothepathologicprogressioninbreast,colorectal,andcervicalcarcinomas.Nonsolidnodulescommonlycontainpremalignantbronchoal-veolarhyperplasia,whilepart-solidnodulesaremorecommonlybronchoalveolarcarcinomaandsolidnod-ulesareinvasiveadenocarcinoma.Asthesizeofanyoftheseradiologictypesofnoduleincreases,theriskofcancerinthenodulealsoincreases.CT-guidedFNAhasbeenagreatadvanceinthediagnosisofsmallpulmonarynodules.Nodules?5mmindiametermaybeamenabletobiopsybythistechnique,dependingontheskillandexperienceoftheradiologistandcytopathologist.WhentheresultofthebiopsyisclearlymalignantorwhenaspecificbenigndiagnosisismadefromtheFNA,manage-mentdecisionsareclear.However,nonspecificbe-nignfindingssuchasinflammation,cellularatypia,bronchoalveolarhyperplasia,blood,bronchialcells,andgranulomawithoutorganismsonspecialstainsmustbeviewedwithsuspicion,andclinicalandradiographicfollow-upareessential.Bycombiningcarefulradiographicfollow-upbyCT,PET,andthejudicioususeofempiricantibioticsandbiopsy,pa-tientsaresparedunnecessarysurgery.Whileade-finitiveanswertothequestionofwhetherCTscreeningreduceslungcancermortalitymaynotbeforthcomingforseveralyears,physicianswillbeincreasinglyaskedtomanagethesmallpulmonarynodulesdiscoveredbyCTinclinicalpractice.
1528References1JemalA,ChuKC,TaroneRE.RecenttrendsinlungcancermortalityintheUnitedStates.JNatlCancerInst2001;93:277–2832FlehingerBJ,KimmelM,MelamedMR.Theeffectofsurgicaltreatmentonsurvivalfromearlylungcancer:impli-cationsforscreening.Chest1992;101:1013–10183FontanaRS,SandersonDR,WoolnerLB,etal.Lungcancerscreening:theMayoprogram.JOccupMed1986;28:746–7504MelamedMR,FlehingerBJ,ZamanMB,etal.Screeningforearlylungcancer:resultsoftheMemorialSloan-KetteringstudyinNewYork.Chest1984;86:44–535TockmanMS.Survivalandmortalityfromlungcancerinascreenedpopulation:theJohnsHopkinsstudy.Chest1986;89:3245–32656KubikA,ParkinDM,KhlatM,etal.Lackofbenefitfromsemi-annualscreeningforcancerofthelung:follow-upreportofarandomizedcontrolledtrialonapopulationofhigh-riskmalesinCzechoslovakia.IntJCancer1990;45:26–337HenschkeCI,McCauleyDI,YankelevitzDF,etal.EarlyLungCancerActionProject:overalldesignandfindingsfrombaselinescreening.Lancet1999;354:99–1058HenschkeCI,NaidichDP,YankelevitzDF,etal.EarlyLungCancerActionProject:initialfindingsonrepeatscreenings.Cancer2001;92:153–1599SoneS,LiF,YangZG,etal.Resultsofthree-yearmassscreeningprogrammeforlungcancerusingmobilelow-dosespiralcomputedtomographyscanner.BrJCancer2001;84:25–3210SoneS,TakashimaS,LiF,etal.Massscreeningforlungcancerwithmobilespiralcomputedtomographyscanner.Lancet1998;351:1242–124511SwensenSJ,JettJR,SloanJA,etal.Screeningforlungcancerwithlow-dosespiralcomputedtomography.AmJRespirCritCareMed2002;165:508–51312SobueT,MoriyamaN,KanekoM,etal.Screeningforlungcancerwithlow-dosehelicalcomputedtomography:anti-lungcancerassociationproject.JClinOncol2002;20:911–92013KanekoM,EguchiK,OhmatsuH,etal.Peripherallungcancer:screeninganddetectionwithlow-dosespiralCTversusradiography.Radiology1996;201:798–80214DiederichS,WormannsD,SemikM,etal.Screeningforearlylungcancerwithlow-dosespiralCT:prevalencein817asymptomaticsmokers.Radiology2002;222:773–78115NewYorkEarlyLungCancerActionProject.Availableat:http://www.NYELCAP.org.AccessedMarch17,200416HenschkeCI.InternationalEarlyLungCancerActionProject.Availableat:http://www.IELCAP.org.AccessedMarch17,200417LillingtonGA,CaskeyCI.Evaluationandmanagementofsolitarymultiplepulmonarynodules.ClinChestMed1993;14:111–11918ZerhouniEA,StilikFP,SiegelmanSS,etal.CTofthepulmonarynodule:acooperativestudy.Radiology1986;160:319–32719HenschkeCI,YankelevitzDF,SmithJP,etal.Screeningforlungcancer:theEarlyLungCancerActionProjectapproach.LungCancer2002;35:143–14820YankelevitzDF,ReevesA,KostisW,etal.Determinationofmalignancyinsmallpulmonarynodulesbasedonvolumetri-callydeterminedgrowthrates:preliminaryresults.Radiology2000;217:251–25621HenschkeCI,YankelevitzDF,MirtchevaR,etal.CTOpinions/Hypotheses
Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
22
2324
25
26
2728
screeningforlungcancer:frequencyandsignificanceofpart-solidandnonsolidnodules.AJRAmJRoentgenol2002;178:1053–1057
VasquezM,FliederD,TravisWD,etal.EarlyLungCancerActionProjectpathologyprotocol.LungCancer2004(inpress)
NoguchiM,MorikawaA,KawasakiM,etal.Smalladenocar-cinomaofthelung.Cancer1995;75:2844–2852
NationalCancerInstitute.NationalCancerInstituteSurveil-lance,Epidemiology,andEndResults(SEER)program2001.Availableat:http://www.seer.cancer.gov.AccessedMarch17,2004
WynderEL,GrahamEA.Tobaccosmokingasapossibleetiologicfactorinbronchogeniccarcinoma:astudyof684provedcases.JAMA1950;143:329–336
HrubecZ,McLaughlinJK.FormercigarettesmokingandmortalityamongUSveterans:a26-yearfollowup,1954–1980.In:BurnsD,GarfinkelL,SametJ,eds.Changesincigarette-relateddiseaserisksandtheirimplicationforpreventionandcontrol.Bethesda,MD:USGovernmentPrintingOffice,1997;501–530
ThunMJ,LallyCA,FlanneryJT,etal.Cigarettesmokingandchangesinthehistopathologyoflungcancer.JNatlCancerInst1997;89:1580–1586
TockmanMS.Otherhostfactorsandlungcancersuscepti-
2930313233
34353637
bility.In:SametJM,ed.Epidemiologyoflungcancer.NewYork,NY:MarcelDekker,1994;397–412
LubinJH,BoiceJDJr,EdlingC,etal.Lungcancerinradon-exposedminersandestimationofriskfromindoorexposure.JNatlCancerInst1995;87:817–827
PaironJC,BrochardP,JaurandMC,etal.Silicaandlungcancer:acontroversialissue.EurRespirJ1991;4:730–744WestcottJL,RaoN,ColleyDP.Transthoracicneedlebiopsyofsmallpulmonarynodules.Radiology1997;202:97–103YankelevitzDF,HenschkeCI,KoizumiJH,etal.CT-guidedtransthoracicneedlebiopsyofsmallsolitarypulmonarynod-ules.ClinImaging1997;21:107–110
GouldMK,MacleanCC,KuschnerWG,etal.Accuracyofpositronemissiontomographyfordiagnosisofpulmonarynodulesandmasslesions:ameta-analysis.JAMA2001;285:914–924
GoldsmithS,KostakogluL.Nuclearmedicineimagingoflungcancer.RadiolClinNorthAm2000;38:511–524
TorringtonKG,KernJD.Theutilityoffiberopticbronchos-copyintheevaluationofthesolitarypulmonarynodule.Chest1993;104:1021–1024
ReichenbergerF,WeberJ,TammM,etal.Thevalueoftransbronchialneedleaspirationinthediagnosisofperipheralpulmonarylesions.Chest1999;116:704–708
KerrKM.Pulmonarypreinvasiveneoplasia.JClinPathol2001;54:257–271
CHEST/125/4/APRIL,20041529
Downloaded from by guest on February 1, 2010
? 2004 American College of Chest Physicians
Managing the Small Pulmonary Nodule Discovered by CT*
Daniel M. Libby, James P. Smith, Nasser K. Altorki, Mark W. Pasmantier,David Yankelevitz and Claudia I. HenschkeChest 2004;125; 1522-1529DOI 10.1378/chest.125.4.1522
This information is current as of February 1, 2010Updated Information& ServicesUpdated Information and services, includinghigh-resolution figures, can be found at:/content/125/4/1522.full.html
This article cites 31 articles, 19 of which can beaccessed free at:/content/125/4/1522.full.html#ref-list-1
This article has been cited by 16 HighWire-hostedarticles:/content/125/4/1522.full.html#related-urls
Freely available online through CHEST open accessoption
Information about reproducing this article in parts(figures, tables) or in its entirety can be found online at: /site/misc/reprints.xhtml
Information about ordering reprints can be found online:/site/misc/reprints.xhtml
Receive free email alerts when new articles cite thisarticle. Sign up in the box at the top right corner of the online article.
Figures that appear in CHEST articles can bedownloaded for teaching purposes in PowerPoint slide format. See any online article figure for directions ReferencesCitationsOpen AccessPermissions & LicensingReprintsEmail alerting serviceImages in PowerPointformat

Downloaded from by guest on February 1, 2010 ? 2004 American College of Chest Physicians
